
The COVID-19 virus entered the United States in early 2020 causing over 600,000 deaths nationwide in just over a year. While the virus itself took its toll on those who contracted it, front-line workers and hospital leaders struggled with mental and compassion fatigue. That is why Laurie Gerdt, Quality and Patient Safety Advisor for the Indiana Hospital Association (IHA), in coordination with the Indiana Division of Mental Health and Addiction’s District 5 Emergency Disaster Mental Health Response team, initiated the REST (Resiliency and Emotional Support Teams) pilot program to combat stress brought on by the COVID-19 response.

During the height of the public health crisis, hospital leaders were in the unenviable position of needing to collect the most current and accurate information to make difficult decisions in a short amount of time. Leaders then communicated those decisions to staff and frontline workers and reported the outcomes of those decisions, usually in a 24-to-48-hour timeframe or less. Gerdt says that these heightened and prolonged stressors contributed to the need for a REST program.
“Cultivating resilience needs a psychologically safe climate to be comfortable giving and receiving feedback, and time and space to foster a good mindset,” Gerdt said. “Developing resilience is what will keep health care leadership effective, efficient, and most importantly, healthy and in-service.”
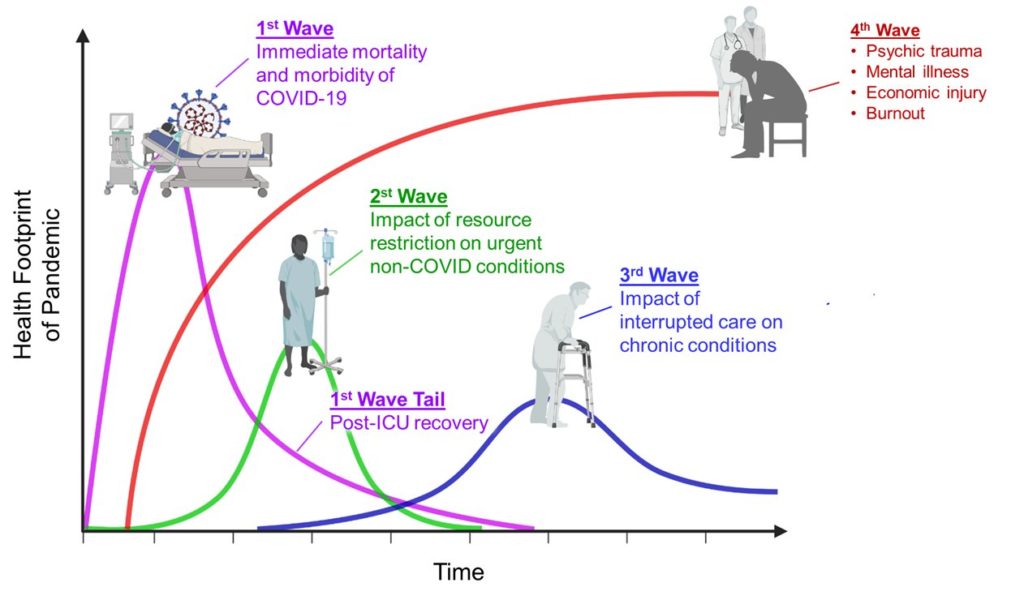
This is of particular importance in light of a projected “fourth wave” of mental health concerns and exhaustion that is expected to come post-pandemic.
The REST pilot program lasted four weeks and consisted of eight sessions, twice a week, with 19 members participating. The program operated on the premise of building resiliency rather than combatting burnout. Gerdt believes this approach is more positive and creates better outcomes.
“There are a lot of resources out there, but we live in a world where a person has to reach out to receive help,” Gerdt said. “Stigma is a huge barrier. We need people to reach in to help instead of waiting on those to reach out. We are all in this crisis together and we know everyone needs help on some level.”
The words, ‘the negative screams at us, but the positive only whispers’ could not be more fitting for the mindset we tried to instill in each participant’s mind. We hope they take those words to heart and can apply it to any future stressors.
-Laurie Gerdt, IHA Quality & Patient Safety Advisor
Erica Prough, director of education and professional practice at Goshen Health, says she appreciates the thoughtfulness behind the pilot program and enjoyed sharing challenges to celebrate successes as well as promoting self-care and support of others.
“Taking 30 minutes each week to meet with peers during the REST sessions has strengthened relationships and provided additional support in times of stress,” Prough said. “As we share our challenges, successes, and how we are caring for ourselves and supporting others, we build resilience and recognize that we are not alone.”
Since the conclusion of the program, Goshen Health has decided to implement the program permanently in their hospital. The hospital leaders have taken their experiences from the pilot and will soon begin offering the program to the entire staff. In addition to the new program, Goshen Health is also looking at potentially hiring a Chief Wellness Officer.
“While proctoring this program, a quote from Barbara Frederickson, a professor at the University of North Carolina at Chapel Hill kept coming to mind,” Gerdt said.
“The words, ‘the negative screams at us, but the positive only whispers’ could not be more fitting for the mindset we tried to instill in each participant’s mind. We hope they take those words to heart and can apply it to any future stressors.”

