Infections happen to everyone. There are infections linked to cuts or toothaches, pneumonia, bladder infections, and cases involving the digestive system. There are bacterial infections, viral infections, and fungal infections. In most cases, with medical intervention or without, our bodies respond effectively to infections.
On some occasions, though, infections lead to sepsis, a condition that kills more people than prostate cancer, breast cancer, and AIDS combined. Sepsis happens when the body’s response to infection results in uncontrolled inflammation that can ultimately damage tissue and organs and can be fatal. In 2019, more than 3,500 Hoosiers died from sepsis.

The story of one 35-year-old Hoosier man shows how dangerous sepsis can be. A tooth infection led to sepsis that, unfortunately, was not controlled quickly enough to avoid liver failure, seizures, and a host of other impacts, including potentially permanent brain damage. “At one point,” his wife recalls, “he said to me, ‘I feel like I’m going to die.’” She said she had never heard of sepsis before her husband experienced it.
I feel like I’m going to die…
– said a patient Experiencing SEPSIS
Fortunately, sepsis is very much on the radar at Indiana hospitals, many of which have launched increasingly effective programs to identify and treat sepsis quickly—and save lives.
According to Rebecca Hancock, Ph.D., CNS, RN, patient safety, and quality advisor for the Indiana Hospital Association, a vital first step in combatting sepsis is raising public awareness. The IHA has designed a Survive Sepsis campaign to get the word out through social media messages and other channels, offering education about what sepsis is, how to recognize it and how to respond.
The IHA and its Indiana Patient Safety Center also work with hospitals across Indiana to create systems of care focusing specifically on sepsis prevention, screening, early identification, and treatment. This includes implementing what is known as “sepsis bundles,” which are evidence-based treatment protocols. These hospital-implemented efforts have had a dramatic and positive impact. Over the course of a decade, hospital sepsis mortality in Indiana dropped from 15 percent to 6 percent.
“In 2015, Terre Haute Regional Hospital began our sepsis management journey by making an organizational commitment to implement specific processes that include early identification of sepsis followed by effective standardized treatment protocols,” says J. Bart Colwell, who chairs the hospital’s board. “Within two years, we received the Joint Commission’s Disease-Specific Certification for Sepsis Care and were the first hospital in the state to achieve this designation.”
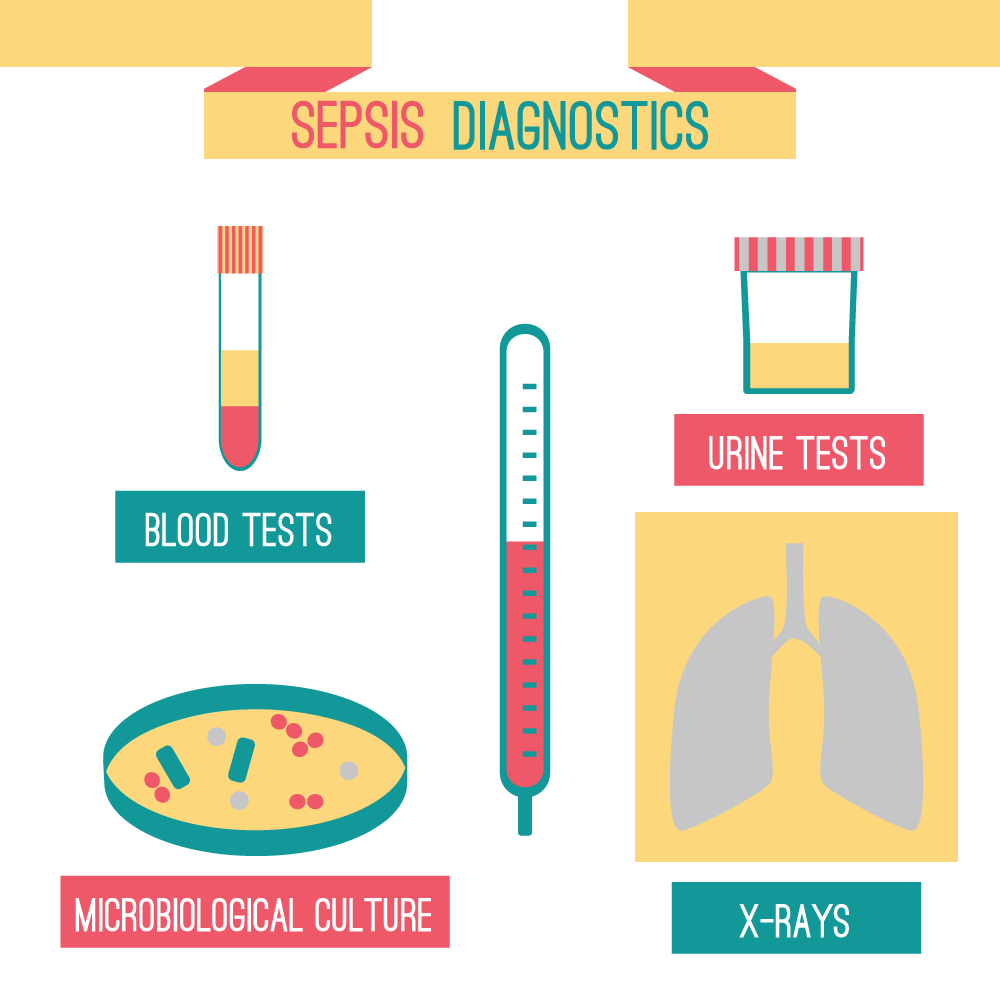
Colwell says the effort aims to identify sepsis early through specific screening tools and follow evidence-based guidelines whenever a patient meets the criteria. It’s not always easy to diagnose sepsis because it shares signs and symptoms with other conditions. That’s why hospitals take such care to screen and monitor for sepsis, watching everything from heart and breathing rates to body temperature to lab test results.
It takes a team to make it happen, Colwell explains. “This good work includes collaboration with physicians, EMS, and post-acute care providers who work with us to continually look for ways to improve,” he says.
Laurie Mustin, RN, director of quality and process improvement at Margaret Mary Health in Batesville, agrees that it takes a collaborative effort to tackle the problem of sepsis. “We have had good engagement, from the board and hospital leadership to the unit level and staff,” she says. The interdisciplinary sepsis team includes her quality and process area, the pharmacy, doctors and nurses, the laboratory, and the information technology department, among others.
The hospital uses performance improvement tools and methodologies to get a handle on sepsis, guided by data and emphasizing education and engagement. Improvement opportunities are shared, successes celebrated, and champions identified to help bring everyone on board. “It’s pretty neat to see how it can make an impact,” Mustin says.

Outside the hospital, what can Hoosiers do about sepsis? To begin with, learn more about the causes and who is most at risk. The IHA’s SurviveSepsis.com website is a great place to start. It is also vital to keep up with vaccinations for such things as flu and pneumonia because those are infections that can lead to sepsis. Other important steps include properly cleaning scrapes and wounds and practicing good hand and oral hygiene. And be vigilant if you have an infection—watch for symptoms including fever, chills, rapid breathing and heart rate, confusion, and disorientation.
As for the patient at the beginning of this story, medical professionals continue to provide treatments, medication, and therapy as he works to recover. Months after sepsis he continues to have difficulty concentrating, has physical limitations, and experiences depression and anxiety. “It is helpful for him to know that some of what he is experiencing is ‘normal’ for those who survive sepsis,” says his wife. “He is a fighter and gets better every day.”

